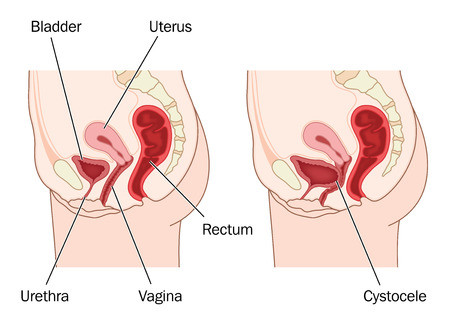
A cystocele can also be called a prolapsed bladder and can occur from excessive straining, such as during heavy lifting, chronic constipation or during childbirth. This condition is common in older women who have given birth to several children.
Cause, Symptoms, Diagnosis of a Prolapsed Bladder
A cystocele develops when the wall between the bladder and a woman’s vagina weakens and the bladder is allowed to fall into the vagina. This condition causes discomfort and problems both during emptying of the bladder and during sexual intercourse. But the problems do not stop there.
Women who have a cystocele also suffer from urine leakage and incomplete emptying of the bladder because of its position inside the vagina. In some cases the opening of the urethra stretches and leakage will occur when any type of pressure is placed upon the bladder, such as when coughing, laughing or sneezing.
During diagnosis the physician will grade the cystocele. Grade 1 is when the bladder drops only a short way, in grade 2 the bladder sinks far enough to reach the opening of the vagina and in grade three the bladder will bulge out through the opening of the vagina.
A secondary condition which places a woman at higher risk for developing a cystocele is the decrease in the hormone estrogen during menopause which has helped to keep the muscles around the vagina strong during the rest of her life. Now, when she has stopped having menstrual periods, the muscles around the vagina and bladder can grow weak. This contributes to the development of a cystocele.
Women who suffer from obesity or are overweight, as well as those who suffer from a chronic cough bronchitis, are also at higher risk for developing a cystocele. Women who have had a hysterectomy may also suffer from a weakness in the pelvic floor while others are born with a genetic connective tissue weakness in the pelvic area which also makes them more susceptible to developing this condition.
If the woman is experiencing difficulty with urination, leakage or pain during sexual intercourse she should seek the advice of her primary care physician or gynecologist. Other symptoms can include a feeling of fullness, and symptoms which increase at the end of standing for long periods during the day. In severe cases the woman will notice a bulge sticking out from the vaginal opening.
A diagnosis of a grade 2 or 3 cystocele can be made from both a description of the symptoms and physical examination. A diagnosis will be confirmed, as well as used for grade 1 cystocele, using a voiding cystourethrogram. This is an x-ray of the bladder that is taken during urination and can show a good picture of what may be blocking the normal flow of urine.
Prolapsed Bladder Treatment
Treatment of a cystocele will be determined based on the severity of the condition, a woman’s age and overall health, the extent of the disease, tolerance for medications as well as the patient’s own opinion or preference.
In mild cases you may not even know you have a cystocele. However, the prolapsed bladder can be uncomfortable, bothersome and sometimes painful. Treatment options for individuals who have mild symptoms may require no treatment or only simple exercises to help strengthen the pelvic floor muscles, such as Kegel exercises.
Other women find it necessary to have a surgical repair done or may use estrogen therapy to increase the strength of the muscles in the pelvic region. In most cases a surgical repair will consist of a vaginal repair and the removal of some of the stretched tissue. Although the results of this type of surgery can last for several years, there is some risk of recurrence because the muscles continue to weaken as you age.
In some cases women may find relief from a vaginal pessary which is a plastic or rubber ring that is inserted into the vagina to support the bladder. These are often used as a temporary alternative to surgery but some women have actually used them for years.
In the meantime the physician may also have some recommendations for ways in which the woman can deal with the urinary incontinence that accompanies a prolapsed bladder. Collagen injections into the urethra can be used to treat incontinence that is caused by a cystocele, but is useless for other types of urinary incontinence. The collagen helps to add bulk and close the gap that allows the urine to leak.
Women are able to help prevent a prolapsed by doing Kegel exercises designed to strengthen the pelvic floor muscles, treat and prevent constipation, avoid heavy lifting, treating a chronic cough or bronchitis and avoiding weight gain.
Herbs Can Help Incontinence
N-Con Tonic is a natural, safe, effective herbal and homeopathic remedy that is a unique formula containing a combination of selected herbs and biochemic tissue salts well known for their toning and strengthening properties on the entire urinary system, prostate and pancreas.
This formula is excellent for the elderly, for women after pregnancy, for people with spinal cord injuries, for stress incontinence and for anyone who has had repeated UTI infections which have weakened bladder functioning.
N-Con Tonic also contains herbs which are well known for their strengthening effect on the immune system and can therefore help to prevent infections of all kinds, including recurring urinary tract infections.
N-Con Tonic is safe to use during and after pregnancy and breastfeeding and will not interact with any other prescription medication. Formulated by our team of experts in natural medicine, N-Con Tonic is pharmaceutically manufactured to the highest standards.
Learn more about N-Con Tonic now.
Why do we promote this?

 Fill out the form below to sign up to our free natural health and healing newsletter and stay up to date on our latest articles about holistic healing therapies and effective home remedies for common ailments. As a thank you for joining our newsletter, we’ll also send you
Fill out the form below to sign up to our free natural health and healing newsletter and stay up to date on our latest articles about holistic healing therapies and effective home remedies for common ailments. As a thank you for joining our newsletter, we’ll also send you